
動物防疫撲殺與人類健康之倫理考量與實務探討
Joyce D' Silva
世界農場動物福利協會慈善大使及前執行長,英國
摘要
人畜共通傳染性疾病(Zoonoses)係指任何能於脊椎動物和人類之間相互感染的疾病,病原體則包括有細菌、寄生蟲、真菌和病毒。近來人類會受到感染的傳染性疾病中,約有75%源自動物或動物性產品,而這些疾病的病原體,則有約60%屬於人畜共通傳染性疾病(Center for Disease Control 2013)。
過去二十年來,SARS、禽流感、豬流感以及其他疾病,蔓延全球各地,由病毒感染而引發的動物疾病,呈現快速增加的趨勢,例如高病原性禽流感病毒株的出現率激增,帶給人類健康嚴重的威脅(Nguyen et al. 2005)。造成動物疾病迅速擴散的原因,許多研究咸認與目前全球工業化畜牧發展有密切關係(Bueckert 2004 in Greger 2006, Webster 2004);此外,載運活體動物與畜牧產品的全球貿易運輸網也提供了最佳傳播途徑(Benun 2006)。
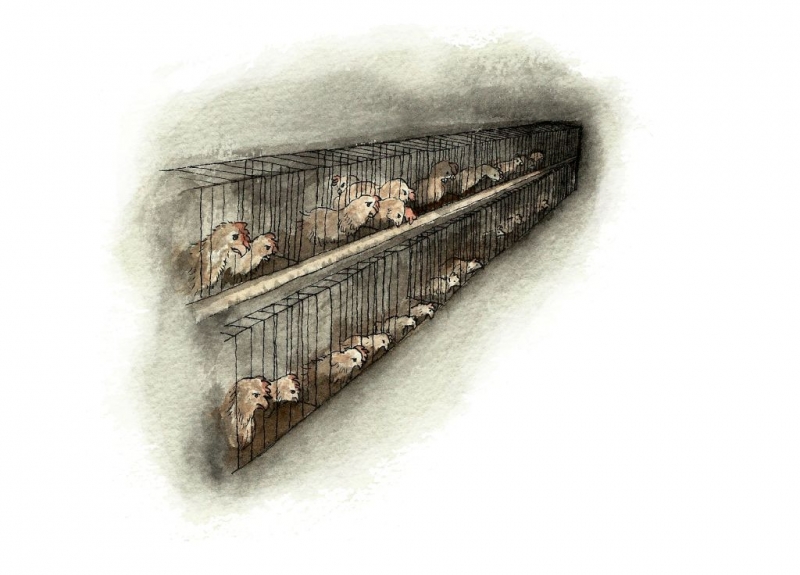
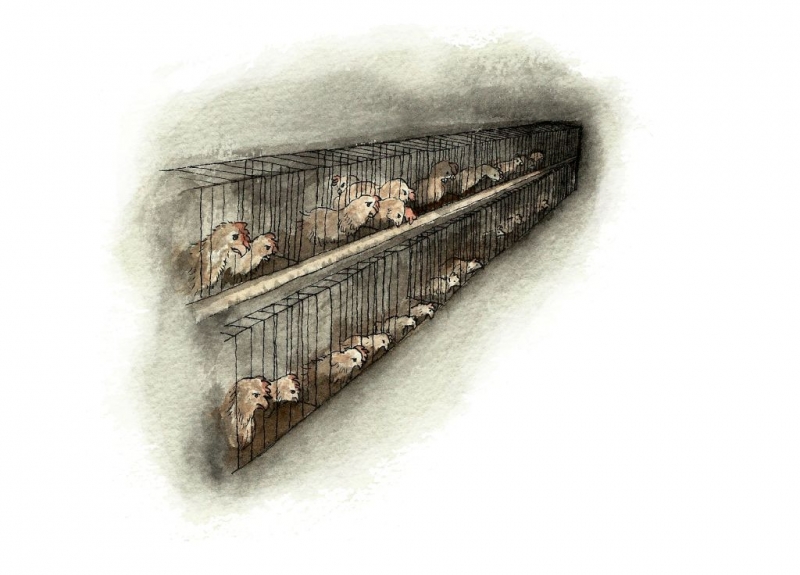
在現代工廠化養雞場裡,成千上萬的雞隻們被塞進擁擠不堪的雞棚裡,牠們可能都是經由系統化育種後挑出的品種,然後再透過非自然的方式被急速增肥。雞隻們面對機械化的控制、育種而產生的壓力,導致免疫功能失調,因此非常容易受到感染 (Rauw et al. 1998)。一旦流感病毒侵入商業家禽養殖場,正好提供了最理想的溫床,讓病毒可以快速地演化、肆虐(Webster and Hulse 2004)。如H5N1型禽流感病毒,即橫掃了亞洲、中東、歐洲和非洲。截至2011年8月,564人被確診感染,其中330人被證實死於禽流感,致命率幾達59%(World Health Organisation 2011)。
禽流感病毒雖然還不至於輕易地傳染給人,但是病毒一旦突變,就可能出現跨物種傳播,爆發全球大規模傳染(Appenzeller 2005)。公共衛生專家們曾經預言,如果爆發流感大流行,將造成全球六千兩百萬人的死亡,而其中又以開發中國家所受的衝擊最為嚴重(C. J. L. Murray et al. 2006)。2002至2003年SARS爆發期間,全球共有8,098個病例,奪走774條人命(National Health Service 2013)。最近一種類似SARS,被稱為MERS(中東呼吸系統症候群)的新型病毒正在中東地區流竄,專家懷疑,MERS冠狀病毒很可能來自豬或蝙蝠。
雖然有其他阻斷疫情擴大的措施,諸如早期檢測、隔離和疫苗接種等,但爆發疫情的地區,多數採大規模撲殺的方式來處理疫情,不只受感染的動物被撲殺,就連無辜的健康動物,往往也遭到池魚之殃,被一併撲殺。而如此忽略動物福利的撲殺方式,更是罔顧世界動物衛生組織OIE提出的人道撲殺規範細則(World Animal Health Organisation 2013)(http://www.oie.int/index.php?id=169&L=0&htmfile=chapitre_1.7.6.htm),即便幾乎全球所有國家都已是世界動物衛生組織的會員國,負有履行其規範之義務。
某些由病毒所引發的疾病如口蹄疫(FMD),帶給人類的威脅其實十分有限,但仍有大批動物,因為經貿理由而難逃被撲殺的命運。1997年台灣爆發口蹄疫,380萬頭豬隻遭到撲殺;2001年英國傳出疫情,為了防止疫情擴大,超過600萬頭牛、羊、豬和山羊被下令撲殺(Extension Disaster Education Network 2013)。這一連串為確保經貿優勢而犧牲健康動物的事證,引發倫理爭議。
本文即將從倫理角度探討疫病的處理相關措施,以期兼顧公共衛生與動物福利雙重考量,同時深入觀察人畜共通傳染病的發生與動物飼養方式之間的關係。
關鍵字:禽流感、疫苗接種、工廠化養殖場、撲殺、眾生
Ethical and Practical Issues regarding Animal Disease, Mass Culling and Human Health
Joyce D Silva
Ambassador and Former Chief Executive for Compassion in World Farming, United Kingdom.
ABSTRACT:
Zoonosesare diseases that can be passed between vertebrate animals and humans. They are caused by all types of pathogenic agents, including bacteria, parasites, fungi, and viruses. Approximately 75% of recently emerging infectious diseases affecting humans are diseases of animal origin; approximately 60% of all human pathogens are zoonotic (Center for Disease Control 2013).
The last two decades have seen a surge in incidence of viral diseases in animals that pose a real threat to human health. SARS, avian and swine flu and other diseases have spread globally. For example, the incidence of highly pathogenic strains of avian influenza has increased dramatically (Nguyen et al. 2005). This spread of animal disease has been linked to the global growth in industrial factory farming (Bueckert 2004 in Greger 2006, Webster 2004) and in some cases to the global trade routes for transporting live animals and animal products (Benun 2006).
In factory farms many thousands of chickens are kept crowded together in each shed. The chickens are likely to be of a uniform breed, selected to grow at an unnaturally fast rate. This causes stress and can make them more vulnerable to infection (Rauw et al. 1998). Once an influenza virus invades a commercial poultry farm, it has an optimum number of susceptible poultry for rapid viral evolution (Webster and Hulse 2004).
TheH5N1 avian flu virus spread across Asia, the Middle East, Europe and Africa. By August 2011, 564 people were confirmed to have been infected, of whom 330 died – a fatality rate of almost 59 per cent (World Health Organisation 2011).
Althoughavian flu does not spread easily to humans as yet, further mutations of the virus could make it easily spreadable and a global pandemic could result (Appenzeller 2005). However, public health experts have estimated that such a flu pandemic could kill as many as 62 million people, mostly in developing countries (C. J. L. Murray et al. 2006).
Duringthe SARS outbreak in 2002-3, there were 8,098 reported cases of SARS in humans and 774 deaths (National Health Service 2013). A similar disease to SARS, known as MERS (Middle East Respiratory Syndrome), is now circulating in that region and is believed to be possibly of pig or bat origin.
Most of these outbreaks of disease have been dealt with by mass culling, not just of infected animals, but of healthy animals too. Often the culling has been undertaken in a manner which totally ignores the welfare of the animals. This is in spite of detailed requirements on humane culling issued by the World Animal Health Organisation, known as the OIE (World Animal Health Organisation 2013) (http://www.oie.int/index.php?id=169&L=0&htmfile=chapitre_1.7.6.htm). Nearly all countries in the world belong to the OIE and have a duty to follow its recommendations.
Otheroptions for dealing with outbreaks include early detection, confinement and separationof infected animals and vaccination strategies.
Some viral diseases, such as foot-and-mouth disease (FMD) have very limited risk to humans, yet animals are still subject to mass culling for economic and trade reasons. During the 1997 FMD outbreak in Taiwan, 3.8 million pigs were destroyed and in the 2001 UK outbreak over 6 million cattle, sheep, pigs and goats were slaughtered to stop the spread of the disease (Extension Disaster Education Network 2013). This raises the ethical issue of killing perfectly healthy animals for trade advantages.
Thispaper will discuss how can we deal with these diseases in an ethical and compassionate manner that protects both public health and the welfare of animals. It will also look at the relationship between these diseases and farming methods.
Keywords: Avian flu (or avian influenza), vaccination, factory farms, culling, sentient beings
The threat to humans from zoonotic diseases
Zoonosesare diseases that can be passed between vertebrate animals and humans. They are caused by all types of pathogenic agents, including bacteria, parasites, fungi, and viruses.Approximately 75% of recently emerging infectious diseases affecting humans are diseases of animal origin and approximately 60% of all human pathogens are zoonotic in origin (Center for Disease Control 2013).
Allfarm animals carry a range of diseases, some of which can infect humans and are therefore zoonotic. Some of these are highly dangerous, such as rabies and anthrax. Some people, such as the very young or very old, those without a spleen or with a transplanted organ, are more vulnerable to zoonotic infection.
The last two decades have seen a surge in the incidence of viral diseases in animals which pose a real threat to human health. Severe acute respiratory syndrome (SARS), avian and swine flu and other diseases have spread globally. For example, the incidence of strains of Highly Pathogenic Avian Influenza (HPAI) has increased dramatically (Nguyen et al. 2005).
SARS is a highly contagious, serious and potentially life-threatening form of pneumonia. During the SARS outbreak in 2002-3, there were 8,098 reported cases of SARS in humans and 774 deaths (National Health Service 2013). This means that the virus killed about 1 in 10 people who were infected. People over 65 years of age were particularly at risk, with over half dying from the infection in this age group. A similar disease to SARS, known as MERS (Middle East Respiratory Syndrome),is now circulating in that region and is believed to be possibly of pig or bat origin.
The H5N1 avian flu virus spread across Asia, the Middle East, Europe and Africa. The World Health Organisation (WHO) reports that from 2003 to 2014, 650 cases of H5N1 have beenreported and 386 people have died from this disease (World Health Organisation 2014). This represents a mortality rate of around 60%.
In2012, 57,500 chickens were culled in areas around Greater Tainan and Changhua County in Taiwan’s first outbreak of the H5N2 avian influenza strain (Taipei Times 2012).
In early 2014, the H7N9 bird flu virus was identified in a Hong Kong market in poultry imported from mainland China and thousands of chickens were culled. The H7N9 virus made the jump from infecting domestic chickens and ducks to infecting people in early 2013. According to the World Health Organisation, cases of human H7N9 infection have been reported so far in China, Hong Kong and Taiwan. By early 2014 there had been morethan 200 cases, with more than 50 deaths (BBC 2014).
Public health experts have estimated that a flu pandemic could kill as many as 62 millionpeople, mostly in developing countries (C. J. L. Murray et al. 2006).
The Nipah virus in pigs affects the respiratory and nervous systems. It is known as porcinerespiratory and neurologic syndrome, porcine respiratory and encephalitic syndrome (PRES), and barking pig syndrome (BPS). It is a highly contagious disease in pigs; however in Bangladesh and India, there have been reports of possible human-to-human transmission of the disease,so precautions are necessary for hospital workers caring for infected patients as well as for workers in slaughterhouses. In humans it causes encephalitis, inflammation of the brain. During an outbreak in Malaysia in 1998-99, over 40% of clinically apparent human cases died (Center for Disease Control 2014).
Recent research has shown that when H5N1 infects humans, it binds to cells in the lower respiratory tract and cannot bind to the trachea (windpipe), with the result that it is not easily spread by sneezing or coughing (Shinya et al. 2006). If mutations were to occur that allowed the virus to bind to cells further up the respiratory tract, the riskof a human pandemicwould suddenly become very immediate.
A dangerous feature of viruses like SARS and Highly Pathogenic Avian Influenza(HPAI) is that they can extend their host range, both within the animal kingdom and sometimes to humans. Although avian flu does not spread easily to humans as yet, further mutations of the virus could make it easily spreadable and a global pandemic could result (Appenzeller 2005). Although most strains of avian flu seem only to infect humans who are in regular close contact with infected animals, there has been a limited (as yet) spread to other humans, usually family members.
A warning was given by a leading expert Ian Mackay, an Associate Professor of Clinical Virology at the University of Queensland in Brisbane: “Each new strain could be one that is better genetically equipped to transmit from person to person. Without contemporary sequence analysis, such a strain could emerge from among the ‘noise’ of human infection by less efficient strains, to begin spreading rapidly and with pandemic potential”( Bloomberg 2014).
There is also the danger that an avian flu virus can infect a pig, mutate and become infectiousto humans in that way. As one of the world’s leading influenza experts, Dr Robert G Webster, has said: “Now we put millions of chickens into a chicken factory, next door toa pig factory and the virus has this opportunity to get in to one of those chicken factories and make billions and billions of these mutations continuously”(Webster,R.G.2008).
Anotherleading US expert has said:
Intensive monitoring of pig viruses is unlikely to come any time soon, however. Most pork-producing countries do not test their pigs at all, and in some that do—such as the U.S.—the testing is done on behalf of the pork producers, who have little economic incentive to share what they find. The reason: pig farmers know pork prices plummet when pigs and flu are linked in the news. In the U.S., government agencies have pieced together a new program they hope will extract badly needed data without threatening the livelihood of producers. But many human health experts fear the compromises made to get pig farmers on board may hobble the effort (Branswell H. 2011).
Why factory farming is implicated in disease spread
This spread of animal disease has been linked to the global growth in industrial factory farming (Bueckert 2004 in Greger 2006, Webster 2004, Lefrançois & Pineau 2014) and insome cases to the global trade routes for transporting live animals and animal products (Benun 2006, Lefrançois & Pineau 2014). Some predict that globalization and ecological disruption will result in the emergence and reemergence of endemic zoonotic diseases (McMichael AJ. 2001).
Let’s look at the animals themselves. Globally, around 58 billion chickens are reared and slaughteredfor meat every year. Around 90% of the breeding stock for those chickens comes from just three companies. The chickens are therefore likely to be of a few uniform breeds, selected to grow at an unnaturally fast rate in order to maximise profits. Many breed lines are developed to reach market weight one day earlier each year (Cruickshank, 2003). Already broiler chickens can grow from fluffy yellow chick to slaughter weight in less thansix weeks. This intensive selective breeding results in genetic uniformity in the population (Delany 2003), so the chickens are likely to be equally vulnerable to the same pathogens, making spread of the virus all the more easy.
A range of studies show that fast growth rates in broilers contribute to leg disorders and to metabolic disorders such as ascites and sudden death syndrome (Knowles et al, 2008). The pain associated with such lameness and other diseases obviously increases the distress endured by the chickens themselves.
In factory farms many thousands of chickens are kept crowded together in each shed. This causes stress, which can make them more vulnerable to infection (Rauw et al. 1998).The more animals that are kept together in a confined space, the higher the virus load generated and consequently, the faster changes in the virus can occur. An intensive poultry farm provides the optimum conditions for viral mutation and transmission - thousands of birds crowded together in a closed, warm and dusty environment is highly conducive to the transmission of a contagious disease.
In time, the result is the emergence of a highly virulent strain of the virus - an HPAI such as H5N1. Once an influenza virus invades a commercial poultry farm, it has an optimum number of susceptible poultry for rapid viral evolution (Webster and Hulse 2004).
The triple impacts of breed, multi-animal confinement and stress/distress, surely make the global intensive chicken industry a pressure cooker for a zoonotic disaster.
Other poultry, pigs, egg-laying hens, beef cattle and dairy cows also suffer from being bred for high productivity and/or being kept in individual confinement or overcrowded indoor conditions.
Across the world, millions of pigs are kept in appalling conditions. Young pigs being fattened up for slaughter are often crowded so closely together that it is almost impossible for all of them to lie down at the same time. They are kept in barren pens, with floors of concrete or bare slats, for excreta to fall through. Being highly intelligent animals, the pigs easily become bored and frustrated and often bite each other’s tails. To prevent this, farmers routinely cut off their tails when they are little piglets. So their bodies are mutilated to make them fit to live in inhumane systems.
Female pigs are often kept in narrow stalls, unable to turn round, throughout their 4 month pregnancies. The European Union has made it illegal to keep pregnant pigs in these narrow sow stalls (gestation crates) for more than 28 days at the start of each pregnancy – after that they must be group-housed (Council Directive 2008/120).
When about to farrow (give birth), the sows are moved to another kind of narrow stall, the farrowing crate, where they give birth and suckle their piglets for about 4 weeks until the piglets are removed to be fattened up. So for most of their lives, the female pigs cannot even turn round. It’s not surprising then that pigs too endure lives of almost permanent discomfort, frustration and distress. Equally it may not be surprising that pigs too are vulnerable to influenza viruses.
The increasing intensification of farming has been linked to the increase in food-borne pathogens, such as E coli, campylobacter, cryptosporidium and listeria (Perry et al. 2013). These infections appear to have little visible impact on the infected animals, but can cause serious, sometimes fatal, results in infected humans.
For example, E coli O157 is a bacterium that lives in the gut of animals, including cattle, sheep, deer and goats. It is also carried by pets and wild birds. It does not normally make the animal ill. In humans, however, the toxins it produces can cause illness ranging from diarrhoea to kidney failure and it is sometimes fatal. It can be found in animal dung. Sometimes animal carcases become contaminated with dung at the slaughterhouse. If meat is not cleaned, handled and cooked properly, humans can become infected.
The increased global movement of people, animals and animal products provides ever more opportunities for the global spread of zoontoic diseases. Although at first, the spread of HPAI was linked to the migratory routes of wild birds, further research has concluded that it is the transport of poultry animals themselves and their products, which has been the main pathway for the spread of this disease (Perry et al. 2013).The spread of H5N1 from China to Europe, Africa and the Middle East correlates with major road and rail routes rather than bird migratory routes or seasons.
Other environmental factors are likely to be affecting the incidence and spread of animal disease. Climate change will have an impact too. Already blue tongue, a disease of sheep, has spread northwards into a warming Europe. Some diseases may thrive in hotter, wetter regions, though others may decrease in increasingly arid conditions.
This disease situation is obviously a serious public health issue, but it has other impacts. Many poor rural families depend on their farm animals for food, income and traction (using them as draught animals, as they cannot afford tractors). Losing their animals to disease represents a financial and sometimes a nutritional crisis. Looked at from the point of view of greenhouse gas emissions (GHGs), then animals who are culled represent a total negative impact, as the GHGs released by them or to produce their food while they were alive, now give no return (Lefrançois & Pineau 2014).
We must ask what the main driver is behind this alarming disease situation. The main finger points to us! Human populations are eating more and more meat and other animal products. The Food and Agriculture Organisation of the United Nations (FAO) has predicted a rough doubling of demand for meat from the year 2000 to 2050 (Steinfeld et al 2006). This change in diet means that more and more animals are being farmed – and the big growth has been in intensive, industrial farming, often known as factory farming. This rapid trend has been called the Livestock Revolution (Delgado et al, 1999).
Dealing with outbreaks/vaccination/culling
Most of these outbreaks of animal disease have been dealt with by mass culling, not just of infected animals, but of healthy animals too. Often the culling has been undertaken in a manner which totally ignores the welfare of the animals. We have seen film of live chickens being packed into sacks to suffocate and of pigs being thrown into pits in the ground where scalding lime has been thrown on top of them, causing a slow and agonising death.
These instances occur in spite of detailed requirements on humane culling issued by the World Animal Health Organisation, known as the OIE (World Animal Health Organisation 2013). This has strict requirements and clearly says: “When animals are killed for disease control purposes, methods used should result in immediate death or immediate loss of consciousness lasting until death; when loss of consciousness is not immediate, induction of unconsciousness should be non-aversive or the least aversive possible and should not cause avoidable anxiety, pain, distress or suffering in animals.” Nearly all countries in the world belong to the OIE and have a duty to follow its recommendations. Sadly it is clear that these requirements are often ignored.
Some viral diseases, such as foot-and-mouth disease (FMD) have very limited risk to humans, yet animals are still subject to mass culling for economic and trade reasons. In animals, the disease can be painful, but it is rarely fatal and the symptoms can be treated. During the 1997 FMD outbreak in Taiwan, 3.8 million pigs were destroyed and in the 2001 UK outbreak over 6 million cattle, sheep, pigs and goats were slaughtered to stop the spread of the disease (Extension Disaster Education Network 2013).
The OIE classifies countries as FMD-free without vaccination, FMD-free with vaccination or, obviously, infected with FMD. Countries where there is an FMD outbreak are subject to stringent controls preventing trade in live animals or meat. As at Feb 2014, Taiwan’s status as FMD-free without vaccination had been suspended. Countries are always keen to attain FMD-free status so that they can continue to trade in animals and their products. This raises the ethical issue of killing perfectly healthy animals for trade advantages.
Options for dealing with disease outbreaks include early detection, confinement and separation of infected animals and vaccination strategies. Veterinary medicine is constantly evolving and there is no doubt that the use of vaccines as preventive medicine has reduced the incidence of several animal diseases, such as Newcastle disease in poultry.
Vaccination, if applied appropriately, could help to prevent further spread of avian influenza from infected to uninfected birds. A number of countries have now implemented avian influenza vaccination strategies.
Vaccinated birds could still become infected with avian influenza, but will show milder symptoms and will be less infectious (with less viral shedding). As a consequence, an AI infection could go unnoticed if all birds are vaccinated. By vaccinating 90% of the birds and with strict monitoring procedures in place, if the flock does become infected with AI, the unvaccinated “sentinel” birds will likely become very ill and die. The European Directive of 2005 on the control of avian influenza also recommended both emergency and preventive vaccination, using a vaccination strategy that incorporates ‘DIVA’ (the ability to Differentiate Infected from Vaccinated Animals) (European Directive 2005/94/EEC).
The USA currently considers vaccination to be one option within its avian influenza management strategy and India is considering its use. China is using avian influenza vaccines widely. The use of vaccination is not universally accepted however and reports suggest that Japan will not use vaccination in a H5N1 outbreak and Hong Kong may cull all poultry if there is an outbreak of this strain.
An increased use of vaccination, rather than widespread culling, has been advocated by the EU’s Scientific Committee on Animal Health and Animal Welfare (EFSA 2006). However, culling remains the main method used by the poultry industry and animal health authorities in Europe.
More humane strategies
Compassion in World Farming believes that:
- Vaccination for avian influenza should be seriously considered for longer-lived birds.
- Vaccination should be used in conjunction with, not as a substitute for, effective monitoring, surveillance and biosecurity measures.
- A ring-fence vaccination procedure should be implemented around an outbreak, to protect uninfected flocks in nearby surroundings.
- Any vaccination procedure should involve the use of sentinel birds to aid monitoring and to prevent infections from ‘hiding’ within a vaccinated flock.
There is a huge burden of responsibility on public bodies and governments to take action to prevent a pandemic of bird flu. The Task Force on the Convention of Migratory Species (CCMS) of the United Nations Environment Programme has stated: “ Governments, local authorities and international agencies need to take a greatly increased role in combating the role of factory farming, commerce in live poultry and wildlife markets, which provide ideal conditions to spread and mutate into a more dangerous form” (UN 2006).
Governments must do all they can to prevent disease outbreaks, they must act swiftly to contain any outbreaks and they must ensure that any culling of animals, which is deemed necessary, is done in the most humane manner possible.
Governments should also end any subsidies to intensive animal farms and encourage and promote more humane and sustainable farming systems, which are more gentle on the animals, respect the environment and support rural livelihoods. The use of wet markets should be discouraged and phased out, with alternatives put in place. Wildlife markets should also be phased out.
For the longer term, governments should advise the population on healthy eating including moving towards a more plant-based diet, and they should consider taxing unhealthy foods such as saturated fats, most of which come from animal foods.
Ethical issues regarding our treatment of animals
We now slaughter over 65 billion animals a year for our food. From an ethical viewpoint, each one of those creatures is an individual sentient being, capable of enjoying life, but all too often enduring only the misery of the factory farm.
Some philosophies and religions, such as Buddhism, regard animals as sentient beings. The European Union (consisting of 28 countries at time of writing) has formally recognised animals as sentient beings in law in the Lisbon Treaty (Lisbon Treaty 2008).
Conscientious consumers either avoid meat, or meat and animal products, becoming vegetarian or vegan, or they purchase only animal products which guarantee high welfare standards, such as free range/pasture-based or high welfare organic standards.
We are all not just consumers, but also citizens. Many conscientious consumers also become active as campaigners for higher welfare standards, for reduced animal transport times and better transport conditions, and for slaughter based on humane principles. They may act individually, lobbying their elected Parliamentarians and local shops, or they may join campaigns run by dedicated groups like Compassion in World Farming, who run campaigns aimed at decision-makers and who also engage with food businesses in order to persuade them to set higher welfare standards for their suppliers.
Of course there can be another good reason to reduce consumption of meat. Over consumption of meat can contribute to diseases like colon cancer, type 2 diabetes and heart disease, all of which are linked also to the growing obesity epidemic. The World Cancer Research Fund recommends: “Limit intake of red meat and avoid processed meat… Eat mostly foods of plant origin” (WCRF/AICR, 2007).Whilst it may be purely in one’s own self-interest and good health to reduce meat consumption, one could also see it as a responsibility to care for one’s health and to reduce the burden on national health care systems.
The major religions and spiritual traditions of the world recommend lives of compassion, charity and peace. It is hard to see how producing and consuming animals reared in industrial ways can be compatible with such ways of life. We need to support food and farming systems which support the livelihoods of smallholder farmers, respect all creatures, and are gentle on the planet.
Reference
AppenzellerT. 2005. Tracking the next killer. National Geographic, October: 2-31.
BanksJ., Speidel E.S., Moore E. et al. 2001. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Archives of Virology 146: 963-973.
BBCNews China. Accessed Jan 28th 2014.
BennunL. 2006. Reality takes wings over bird flu. BBC News (online). 17 February 2006. Available at: http://news.bbc.co.uk/1/hi/sci/tech/4721598.stm
Bloombergwebsite. Accessed Feb 14 2014 (by Jason Gale)
BranswellH, 2011. Flu Factories: The next pandemic virus may be circulating on U.S. pig farms, but health officials are struggling to see past the front gate. Scientific American Jan 2011
Bueckert2004 in: Greger, M. 2006. Avian Influenza: Unjustly Blaming Outdoor Flocks.
TheLancet. 2006. Global avian Influenza controls must be scaled up now. The Lancet 367: 184. Available at:http://www.hsus.org/farm/news/ournews/avian_flu_free_range.html.
Centerfor Disease Control website as at Nov. 2013,http://www.cdc.gov/ncezid/.
Centerfor Disease Control website as at 2/3/14:Hendra Virus Disease and Nipah Virus Encephalitis.
CouncilDirective 2005/94/EC of 20 December 2005 on Community measures for the control of avian influenza and repealing Directive 92/40/EEC.
CouncilDirective 2008/120 on the welfare of pigs.
Cruickshank, G., 2003. Cobb focuses on bottom line performance. Poultry World July 2003, p.22.
Delany, M.N. 2003. Genetic Diversity and Conservation of Poultry. In: Muir, W.M. and Aggrey, S.E. (eds). Poultry Genetics, Breeding and Biotechnology, CABI Publishing, UK, pp.257-281.
DelgadoC, Rosegrant M, Steinfeld H, Ehui S, Courbois C (1999) Livestock to 2020. The Next Food Revolution. Food, Agriculture and the Environment Discussion Paper 28 (IFPRI, Washington, DC).
European Food Safety Authority (EFSA). 2006 EFSA Scientific Report of the Scientific Panelon Biological Hazards on: Food as a possible source of infection with highly pathogenic avian influenza viruses for humans and other mammals. EFSA Journal. 74, 1-29; 2006.http://www.efsa.europa.eu/EFSA/Scientific_Document/biohaz_report_ej74_avian_influenza_en2.pdf.
ExtensionDisaster Education Network website. Accessed at Nov 2013: http://eden.lsu.edu/TOPICS/AGDISASTERS/FMD/Pages/default.aspx.
Knowles, T. G., Kestin, S. C., Haslam, S. M., Brown, S. N., Green, L. E., Butterworth, A., Pope, S. J., Pfeiffer, D. and Nicol, C. J., 2008. Leg disorders in broiler chickens: prevalence, risk factors and prevention. Plos one 3 (2): e1545. doi: 10.1371/journal.pone.0001545.
LefrançoisT. & Pineau T. 2014. Public health and livestock: Emerging diseases in food animals. Animal Frontiers. 4(1):4-6.
LisbonTreaty 2008. Consolidated Version of the Treaty on the Functioning of the European Union art. 13, 2008 Official Journal C 115. http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:C:2008:115:0047:0199:en:PDF
McMichaelAJ (2001) Human culture, ecological change, and infectious disease: Are we experiencing history’s fourth great transition? Ecosystem Health 7:107-115.
Murray C. J. L. et al., Estimation of potential global pandemic influenza mortality on the basisof vital registry data from the 1918-20 pandemic: a quantitative analysis, Lancet 368 (2006), pp. 2211-18.
NationalHealth Service UK website. Accessed Nov 2013: (http://www.nhs.uk/ Conditions/SARS/Pages/Introduction.aspx).
NguyenD.C., Uyeki T.M., Jadhao S. et al. 2005. Isolation and characterization of Avian Influenza Viruses, Including Highly Pathogenic H5N1, from Poultry in Live Bird, Markets in Hanoi, Vietnam, in 2001.Journal of Virology 79(7): 4201-4212.
PerryB.D., Grace D., Sones K., 2013. Current drivers and future directions of global livestock disease dynamics. PNAS 110, 52: 20871-20877.
RauwW. M., Kanis E., Noordhizen-Stassen E.N., Grommers F.J. 1998. Undesirable side effects of selection for high production efficiency in farm animals; a review. Livestock Production Science 56: 15-33.
ShinyaK., Ebina M., Yamada S., Ono M., Kasai N. and Kawaoka Y. 2006. Avian flu: Influenza virus receptors in the human airway. Nature 440: 435-436.
Steinfeld, H et al, 2006. Livestock’s Long Shadow: Environmental issues and options. FAO, Rome.
TaipeiTimes 4 March 2012, quoting the Council of Agriculture (COA).
UnitedNations homepage. Accessed at 30/9/06.
Webster, R.G. 2004 Wet markets – a continuing source of severe acute respiratory syndrome and influenza? The Lancet 363: 234-36.
WebsterR.G. and Hulse D.J. 2004. Microbial adaptation and change: avian influenza.Revue Scientifique et Technique23(2): 453-465.
WebsterR,G. 2008. Quoted in the DVD “Pandemic Prevention”, HSUS.
WorldAnimal Health Organisation (OIE) website. Accessed at Nov 2013: Terrestial Animal Health Code. Chapter 7.6. Killing of animals for disease control purposes, Article 7.6.1. http://www.oie.int/index.php?id=169&L=0&htmfile=chapitre_1.7.6.htm.
WCRF/AICR, 2007.Food, nutrition, physical activity and the prevention of cancer: A global perspective, World Cancer Research Fund/American Institute for Cancer Research, Washington DC. http://www.dietandcancerreport.org/cancer_resource_center/downloads/Second_Expert_Report_full.pdf.
WorldHealth Organisation website. Accessed 27/2/14): http://www.who.int/influenza/human_animal_interface/EN_GIP_20140124CumulativeNumberH5N1cases.pdf?ua=1.